Support, Solutions & Hope for Patients and Caregivers
If you or your loved one is living with or showing signs of hypothalamic obesity, you’re not alone and there is help.
The Raymond A. Wood Foundation (RAWF) is dedicated to improving the lives of survivors of hypothalamic-pituitary brain tumors and the complex challenges that can follow, including hypothalamic obesity (HO).

What Is Hypothalamic Obesity?
Hypothalamic obesity, also known as acquired hypothalamic obesity, is a rare and serious condition that can develop after damage to the hypothalamus often caused by surgery, radiation, or treatment for a brain tumor like craniopharyngioma. The hypothalamus is responsible for regulating hunger, metabolism, and energy balance. When it’s impaired, the body may begin storing fat rapidly, no matter how much a person eats or exercises.
Many individuals with hypothalamic obesity experience hyperphagia which is a relentless, uncontrollable sense of hunger and food preoccupation, where thoughts about food dominate daily life. These symptoms can be overwhelming and emotionally draining for both patients and caregivers.
This isn’t about willpower or lifestyle changes.
Hypothalamic obesity is a medical condition that deserves recognition, research, and access to better treatments.
Stay Connected with HO News & Resources
Get monthly insights on research updates, clinical trials, education events, and community support — straight to your inbox.
The Impact of Hypothalamic Obesity: More than Weight Gain
Hypothalamic obesity is not just about weight. It’s a complex, chronic condition that affects nearly every part of life. The rapid and persistent weight gain can lead to serious health complications, including type 2 diabetes, heart disease, sleep apnea, liver problems, and reduced mobility.
Beyond the physical impact, the emotional toll is profound. Patients often face stigma, misdiagnosis, and frustration when typical weight-loss approaches don’t work. The constant hunger, food preoccupation, and sense of losing control over one’s body can lead to anxiety, depression, and social isolation.
For caregivers and families, the condition can be incredibly difficult to manage. Watching a loved one struggle while navigating a healthcare system that often doesn’t understand hypothalamic obesity can leave families feeling helpless and unheard.
Despite how serious it is, hypothalamic obesity remains under-recognized and under-treated. That’s why advocacy, research, and community support are essential.
Support for Patients and Families Navigating HO
At the Raymond A. Wood Foundation, we support patients and families navigating hypothalamic obesity and the challenges that come with it through:
Patient-Centered Research
We lead and support research grounded in real patient experiences. Through our Hypothalamic-Pituitary Brain Tumor Patient Registry, we collect critical data that helps shape clinical care and drives new treatment development.
Collaboration with Industry & Clinicians
We work with pharmaceutical and biotech companies and clinical researchers working to develop therapies for hypothalamic obesity, advocating for trials and treatment pathways that reflect the realities of patients’ lives.
Policy & Insurance Advocacy
We advocate for insurance coverage of emerging therapies like GLP-1s and Setmelanotide, while raising awareness among healthcare providers and policymakers about the complexity of hypothalamic obesity.
Education & Care Management Resources
We provide plain-language, accessible education on managing hypothalamic obesity and its related symptoms with the aim of empowering patients and caregivers to advocate for better care.
Community Support & Connection
From live webinars to private support groups, we create safe, supportive spaces where patients and caregivers can connect, share experiences, and find strength in community.
Innovation in Monitoring Tools
We’re developing the at-home sodium meter, a groundbreaking device to help survivors manage critical health needs from home, improving safety and independence.
Resources
Whether you’re newly navigating hypothalamic obesity or looking for deeper understanding, our resource library offers trusted tools to support your journey. Below are links to explore expert-led presentations, published research, recommended books, and educational articles. You can also visit our YouTube channel for recorded webinars and stories from the community, or explore on-demand learning on our Uscreen platform.
Hypothalamic Obesity: Clinical Management and Nutritional Approaches
This powerful session, led by Dr. Jennifer Miller (University of Florida pediatric endocrinologist) and Michael Tan (registered dietitian and CDE), dives deep into the science and lived experience of hypothalamic obesity (HO). Dr. Miller explains how hypothalamic injury disrupts hunger and fullness signaling, leading to hyperinsulinemia, sweet taste dysregulation, and relentless weight gain. Michael Tan offers clear, compassionate guidance on building meals that support metabolic balance—eliminating sweet taste, understanding the role of insulin, and reducing food focus without shame. They challenge common assumptions about fruit, artificial sweeteners, and carbs, while acknowledging the emotional and sensory complexities families face. Dr. Miller also provides an up-to-date review of current and emerging medications—what has worked, what hasn’t, and the promising future of therapies like setmelanotide. Grounded in research and real family stories, this session is a must for anyone navigating HO care.
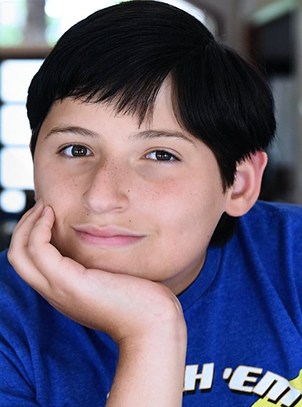
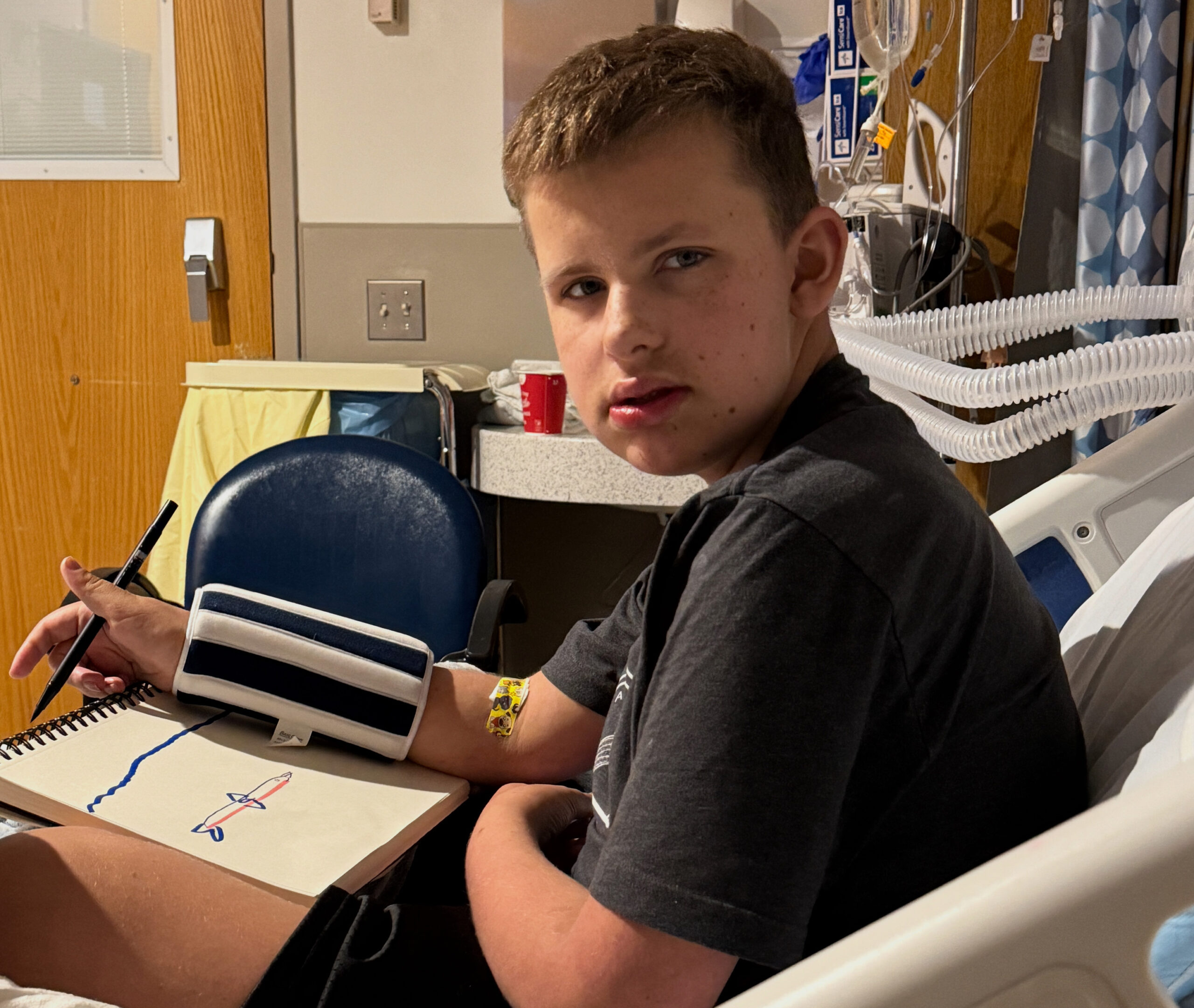
View more presentations on HO and other related conditionsHope for HO – a mother shares her experiences in finding a solution for her son’s HO.
HO Clinical Trials Panel – a recent panel of principle investigators on promising treatments for HO.
Hungry for Solutions, Marci Serota, RDN This book was written by a mother and registered dietician sharing her quest to find solutions for her son with HO.
Would You Know How to Recognize and Treat Hypothalamic Obesity?
Marci Serota, RDN with Eugenie Hsu, PhD and Shana McCormack, MD, MTR
Feasibility, safety, and efficacy of dietary or lifestyle interventions for hypothalamic obesity: A systematic review.
Van Roessel IMAA, Van Den Brink M, Dekker J, Ruitenburg-van Essen BG, Tissing WJE, van Santen HM. Clin Nutr. 2024 May 27;43(8):1798-1811. doi: 10.1016/j.clnu.2024.05.028. Online ahead of print. PMID: 38955055
Zhang Q, Feng Y, Wu D, Xie Y, Wu G, Wu W, Wang H, Liu X, Fan L, Xiang B, Sun Q, Li Y, Wang Y, Ye H. Serum Metabolomic and Lipidomic Profiling Reveals the Signature for Postoperative Obesity among Adult-Onset Craniopharyngioma. Metabolites. 2024 Jun 17;14(6):338. doi: 10.3390/metabo14060338. PMID: 38921473; PMCID: PMC11205291.
Beckhaus J, Eveslage M, Bison B, Friedrich C, Müller HL. Impact of parental body mass index at diagnosis on obesity in survivors of pediatric craniopharyngioma. Endocr Connect. 2024 Jun 1:EC-24-0126. doi: 10.1530/EC-24-0126. Epub ahead of print. PMID: 38904467.
Müller HL, Zhou J, Peng J. Editorial: Recent advances in pediatric craniopharyngioma. Front Endocrinol (Lausanne). 2024 Apr 19;15:1413744. doi: 10.3389/fendo.2024.1413744. PMID: 38706703; PMCID: PMC11066279.
Roth CL, Scimia C, Shoemaker AH, Gottschalk M, Miller J, Yuan G, Malhotra S, Abuzzahab MJ. Setmelanotide for the treatment of acquired hypothalamic obesity: a phase 2, open-label, multicentre trial. Lancet Diabetes Endocrinol. 2024 Jun;12(6):380-389. doi: 10.1016/S2213-8587(24)00087-1. Epub 2024 Apr 30. PMID: 38697184.
Tena-Sempere M. Setmelanotide: new promise for the treatment of hypothalamic obesity? Lancet Diabetes Endocrinol. 2024 Jun;12(6):366-367. doi: 10.1016/S2213-8587(24)00109-8. Epub 2024 Apr 30. PMID: 38697183.
Rovani S, Butler V, Samara-Boustani D, Pinto G, Gonzalez-Briceno L, Nguyen Quoc A, Vermillac G, Stoupa A, Besançon A, Beltrand J, Thalassinos C, Flechtner I, Dassa Y, Viaud M, Arrom-Branas MB, Boddaert N, Puget S, Blauwblomme T, Alapetite C, Bolle S, Doz F, Grill J, Dufour C, Bourdeaut F, Abbou S, Guerrini-Rousseau L, Leruste A, Beccaria K, Polak M, Kariyawasam D. Long-term weight gain in children with craniopharyngioma. Eur J Endocrinol. 2024 May 2;190(5):363-373. doi: 10.1093/ejendo/lvae044. PMID: 38662730.
Tsumori M, Itonaga T, Oyake M, Hirano N, Oyama N, Ihara K. Infantile Hypothalamic Hamartoma: A Rare Presentation of Isolated Obesity. JCEM Case Rep. 2024 Mar 19;2(3):luae033. doi: 10.1210/jcemcr/luae033. PMID: 38505090; PMCID: PMC10948354.
Chartoumpekis DV, Habeos EE, Psilopanagioti A. Evaluating the effectiveness and underlying mechanisms of incretin-based treatments for hypothalamic obesity: A narrative review. Obes Pillars. 2024 Feb 24;10:100104. doi: 10.1016/j.obpill.2024.100104. PMID: 38463533; PMCID: PMC10924130.
Roth CL, McCormack SE. Acquired hypothalamic obesity: A clinical overview and update. Diabetes Obes Metab. 2024 Apr;26 Suppl 2:34-45. doi: 10.1111/dom.15530. Epub 2024 Mar 7. PMID: 38450938.
Gatta-Cherifi B, Mohammedi K, Cariou T, Poitou C, Touraine P, Raverot G, Brue T, Chanson P, Illouz F, Grunenwald S, Chabre O, Sonnet E, Cuny T, Bertherat J, Czernichow S, Frison E, Tabarin A. Impact of exenatide on weight loss and eating behavior in adults with craniopharyngioma-related obesity: the CRANIOEXE randomized placebo-controlled trial. Eur J Endocrinol.
Pereira Neto B, Pais Cunha I, Leite-Almeida AL, Ferreira S, Coelho J, Lago R, Pereira J, Gil-da-Costa MJ, Almeida P, Castro-Correia C. Quality of Life and Hormonal Impairment in Pediatric Patients With Craniopharyngiomas. Cureus. 2024 Jan 20;16(1):e52621. doi: 10.7759/cureus.52621. PMID: 38374867; PMCID: PMC10875977.
Ng VWW, Gerard G, Koh JJK, Loke KY, Lee YS, Ng NBH. The role of glucagon-like peptide 1 receptor agonists for weight control in individuals with acquired hypothalamic obesity-A systematic review. Clin Obes. 2024 Jun;14(3):e12642. doi: 10.1111/cob.12642. Epub 2024 Jan 25. PMID: 38273176.
van Santen HM, Denzer C, Müller HL. Could setmelanotide be the game-changer for acquired hypothalamic obesity? Front Endocrinol (Lausanne). 2024 Jan 4;14:1307889. doi: 10.3389/fendo.2023.1307889. PMID: 38239988; PMCID: PMC10794340.
Gan HW, Cerbone M, Dattani MT. Appetite- and Weight-Regulating Neuroendocrine Circuitry in Hypothalamic Obesity. Endocr Rev. 2024 May 7;45(3):309-342. doi: 10.1210/endrev/bnad033. PMID: 38019584; PMCID: PMC11074800.
Roth CL, Zenno A.Treatment of hypothalamic obesity in people with hypothalamic injury: new drugs are on the horizon. Front Endocrinol (Lausanne). 2023 Sep 13;14:1256514. doi: 10.3389/fendo.2023.1256514. PMID: 37780616; PMCID: PMC10533996.
Hu HZ, Lei L. Bariatric surgery for hypothalamic obesity in patients with craniopharyngioma: A literature review. Asian J Surg. 2023 Dec;46(12):5479. doi: 10.1016/j.asjsur.2023.07.117. Epub 2023 Aug 1. PMID: 37537035.
Dassen AR, van Schaik J, van den Munckhof P, Schuurman PR, Hoving EW, van Santen HM. Could deep brain stimulation be a possible solution for acquired hypothalamic obesity? Heliyon. 2023 Mar 9;9(3):e14411. doi: 10.1016/j.heliyon.2023.e14411. PMID: 36967879; PMCID: PMC10036662
Sciacovelli C, Moschione G, Garelli S, Pagotto U. Semaglutide for Treating Obesity Induced by Craniopharyngioma Resection: A Successful Case Study. JCEM Case Rep. 2023 Jul 27;1(4):luad074. doi: 10.1210/jcemcr/luad074. PMID: 37908981; PMCID: PMC10580492.
Yousuf OK, Salehani A, Zimmerman K, Estevez-Ordonez D, Madura C, Arynchyna-Smith A, Johnston JM, Rozzelle CJ, Rocque BG, Blount JP. Does subtotal resection ameliorate hypothalamic morbidity in pediatric craniopharyngioma? A 30-year retrospective cohort study. J Neurosurg Pediatr. 2023 Aug 11;32(5):569-575. doi: 10.3171/2023.5.PEDS22568.
van Roessel IMAA, de Graaf JP, Biermasz NR, Charmandari E, van Santen HM. Acquired hypothalamic dysfunction in childhood: ‘what do patients need?’ – an Endo-ERN survey. Endocr Connect. 2023 Sep 13;12(10):e230147. doi: 10.1530/EC-23-0147. PMID: 37531603; PMCID: PMC10503223.
Kayadjanian N, Hsu EA, Wood AM, Carson DS. Caregiver Burden and Its Relationship to Health-Related Quality of Life in Craniopharyngioma Survivors. J Clin Endocrinol Metab. 2023 Dec 21;109(1):e76-e87. doi: 10.1210/clinem/dgad488. PMID: 37597173; PMCID: PMC10735386.
Van Schaik J, Schouten-van Meeteren AYN, Vos-Kerkhof E, Janssens GO, Porro GL, Fiocco M, Bakker B, Tissing WJE, Hoving EW, van Santen HM. Treatment and outcome of the Dutch Childhood Craniopharyngioma Cohort study: First results after centralization of care. Neuro Oncol. 2023 Dec 8;25(12):2250-2261. doi: 10.1093/neuonc/noad112. PMID: 37381692; PMCID: PMC10708930.
Schultes B, Ernst B. Long-term outcomes after gastric bypass surgery in patients with craniopharyngioma-related hypothalamic obesity-Three cases with 7, 8, and 14 years follow-up. Obes Res Clin Pract. 2023 Jul-Aug;17(4):361-365. doi: 10.1016/j.orcp.2023.06.004. Epub 2023 Jun 26. PMID: 37380506.
Hinton EC, Lithander FE, Elsworth RL, Hawton K, Narayan K, Szymkowiak S, Bedford HL, Naeem N, Elson R, Taylor-Miller T, Hamilton-Shield JP, Crowne EC. Evaluating Eating Behaviour, Energy Homeostasis, and Obesity in Childhood-Onset Craniopharyngioma: A Feasibility Study. Horm Res Paediatr. 2024;97(1):80-93. doi: 10.1159/000530863. Epub 2023 May 17. PMID: 37231854; PMCID: PMC10777714
McCormack SE, Wang Z, Wade KL, Dedio A, Cilenti N, Crowley J, Plessow F, Bamba V, Roizen JD, Jiang Y, Stylli J, Ramakrishnan A, Platt ML, Shekdar K, Fisher MJ, Vetter VL, Hocking M, Xiao R, Lawson EA. A Pilot Randomized Clinical Trial of Intranasal Oxytocin to Promote Weight Loss in Individuals With Hypothalamic Obesity. J Endocr Soc. 2023 Mar 17;7(5):bvad037. doi: 10.1210/jendso/bvad037. PMID: 37153702; PMCID: PMC10154909.
Beckhaus J, Friedrich C, Boekhoff S, Calaminus G, Bison B, Eveslage M, Timmermann B, Flitsch J, Müller HL. Outcome after pediatric craniopharyngioma: the role of age at diagnosis and hypothalamic damage. Eur J Endocrinol. 2023 Mar 2;188(3):lvad027. doi: 10.1093/ejendo/lvad027. PMID: 36857103
Rachmasari KN, Strauss SB, Phillips CD, Lantos JE, An A, Cisse B, Ramakrishna R, Schwartz TH, Dobri GA. Posterior hypothalamic involvement on pre-operative MRI predicts hypothalamic obesity in craniopharyngiomas. Pituitary. 2023 Feb;26(1):105-114. doi: 10.1007/s11102-022-01294-0. Epub 2022 Dec 3. PMID: 36462067.
Shoemaker AH, Tamaroff J. Approach to the Patient With Hypothalamic Obesity. J Clin Endocrinol Metab. 2023 Apr 13;108(5):1236-1242. doi: 10.1210/clinem/dgac678. PMID: 36413492; PMCID: PMC10306088.
Craven M, Crowley JH, Chiang L, Kline C, Malbari F, Hocking MC, McCormack SE. A Survey of Patient-Relevant Outcomes in Pediatric Craniopharyngioma: Focus on Hypothalamic Obesity. Front Endocrinol (Lausanne). 2022 May 9;13:876770. doi: 10.3389/fendo.2022.876770. PMID: 35615720; PMCID: PMC9124861.
Oxytocin and Naltrexone Successfully Treat Hypothalamic Obesity in a Boy Post-Craniopharyngioma Resection
Eugenie A Hsu, Jennifer L Miller, Francisco A Perez, Christian L Roth
Hypothalamic Obesity: Prologue and Promise
Abuzzahab M.J.a, Roth C.L.b, Shoemaker A.H.c
A Pilot Randomized Clinical Trial of Intranasal Oxytocin to Promote Weight Loss in Individuals With Hypothalamic Obesity
Shana E McCormack, Zi Wang, Kristin L Wade, Anna Dedio, Nicolette Cilenti, Julia Crowley, Franziska Plessow, Vaneeta Bamba, Jeffrey D Roizen, Yaoguang Jiang, Jack Stylli, Arjun Ramakrishnan, Michael L Platt, Karuna Shekdar, Michael J Fisher, Victoria L Vetter, Matthew Hocking, Rui Xiao, Elizabeth A Lawson
Help Shape the Future of HO Care
Join Our Patient Registry
Your voice is crucial in addressing the challenges of hypothalamic obesity and hyperphagia! Join us in shaping the future of research by enrolling in the Hypothalamic Pituitary Brain Tumor Patient Registry. Your participation, at your own pace, will contribute valuable insights to better understand and treat these conditions

Clinical Trials in Acquired Hypothalamic Obesity
Looking for information on all current clinical trials for hypothalamic obesity? Visit our Clinical Trial Finder on our website to explore the latest research opportunities and advancements
Clinical Trial FinderHypothalamic Obesity News
Hypothalamic Syndrome: Finally, a Way to Describe What We’ve Been Living

New Frontiers in Hypothalamic Obesity Research
Updates on Current and Pending Hypothalamic Obesity Clinical Trials

Raymond A. Wood Foundation Partners with STOP Obesity Alliance
Support Our Work
The Raymond A. Wood Foundation advocates for survivors and caregivers faced with challenges after brain tumor treatment. A donation — big or small — helps us do this important work.

