For Clinicians, Researchers, and Industry Partners Working to Advance Care in Acquired Hypothalamic Obesity
At the Raymond A. Wood Foundation (RAWF), we support patients and caregivers living with hypothalamic obesity which is a rare, under-recognized condition resulting from hypothalamic damage. We don’t provide clinical care, but we offer trusted support to the community and create opportunities for researchers and innovators to engage with patient experience, real-world data, and advocacy.
This page is designed for healthcare professionals, academic researchers, and industry partners who want to understand how we support patients and how we can collaborate to advance care, improve quality of life, and accelerate research in HO.
Understanding the Patient and Caregiver Experience
For many clinicians, acquired hypothalamic obesity (HO) is seen primarily as treatment-resistant weight gain. But for patients and families, the reality is far more complex and deeply distressing.
The weight gain is just the surface. Underneath are the relentless symptoms that profoundly affect daily life:
- Hyperphagia: An uncontrollable, insatiable hunger that persists even after eating.
- Food Preoccupation: Constant thoughts about food can disrupt learning, work, and relationships, especially for children and adolescents.
- Emotional Distress: The combination of physical changes, lack of control, intense and insatiable hunger and social stigma often leads to behavioral issues, depression, anxiety, and isolation.
- Family Strain: Caregivers must manage nutrition, safety, and behavior while advocating for care in systems that often don’t understand the condition.
- Social Isolation: Open access to food, stigma, misunderstanding, and behavioral challenges can lead patients and caregivers to withdraw from school, social events, and even extended family life.
- Lack of Treatment Recognition: Many patients are told to simply “eat less and exercise more” which is advice that not only fails but compounds shame and hopelessness.
In our study, Caregiver Burden and Its Relationship to Health-Related Quality of Life in Craniopharyngioma Survivors (PMID: 37597173), hyperphagia emerged as one of the most burdensome symptoms affecting quality of life. This is not simply a weight issue rather it’s a neurologically driven, life-altering condition that demands deeper understanding, compassionate care and treatment options.
What RAWF Offers the Patient Community
At the Raymond A. Wood Foundation, we support patients and families navigating hypothalamic obesity and the challenges that come with it through:
We provide holistic, real-world support to individuals and families navigating HO, including:
Advocacy: Working to improve access to emerging therapies and educate clinicians and payers on the complexity of HO.
Navigation & Education: Accessible resources to help families understand and manage HO symptoms like hyperphagia, fatigue, and metabolic changes.
Community Support: Caregiver-led support groups, webinars, and peer connections that reduce isolation and foster empowerment.
Technology Innovation: Development of tools like our at-home sodium meter to help patients manage long-term health risks.
Key Data: What Patients Are Telling Us
In our 2023 Caregiver Burden Study, hyperphagia emerged as the top quality-of-life challenge faced by families managing acquired HO. This constant and distressing hunger not only affects physical health but contributes to emotional strain, caregiver burnout, and social withdrawal. Read the full study »
Opportunities to Engage with RAWF
We invite clinicians and researchers to connect with our community and tools:
Patient Registry
Our global Hypothalamic-Pituitary Brain Tumor Patient Registry collects real-world, longitudinal data that can support both clinical care improvements and research efforts.
Learn more or inquire about collaboration
Clinical Trial Finder
We offer a user-friendly Clinical Trial Finder on our website that aggregates relevant clinical trials for acquired hypothalamic obesity and related hypothalamic-pituitary tumors and conditions. Designed with patients and caregivers in mind, this tool simplifies complex trial databases into accessible, filterable results to help families identify potential opportunities for participation and care.
Explore the Clinical Trial Finder
Conference Presentations & Talks
We regularly present data on the latest treatments, research, patient experience, caregiver burden, and innovation. If you’re interested in presenting, viewing or featuring our content, please reach out.
Collaboration Opportunities
RAWF welcomes inquiries from clinical researchers, pharmaceutical and biotech companies, and trial sponsors who want to better engage with patients, recruit for studies, or include patient voice in trial design. Contact us to inquire.
Additional Resources
Video Learning Platform: On-demand educational content for patients and caregivers
YouTube Channel: Webinars, patient stories, and caregiver discussions
Rhythm Pharmaceuticals HO Resource Page: For additional context on acquired HO and treatment development
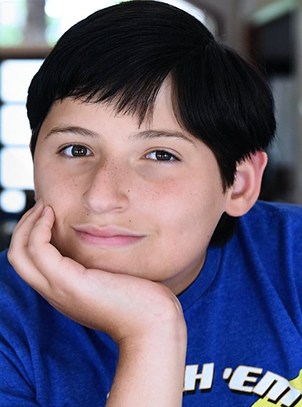
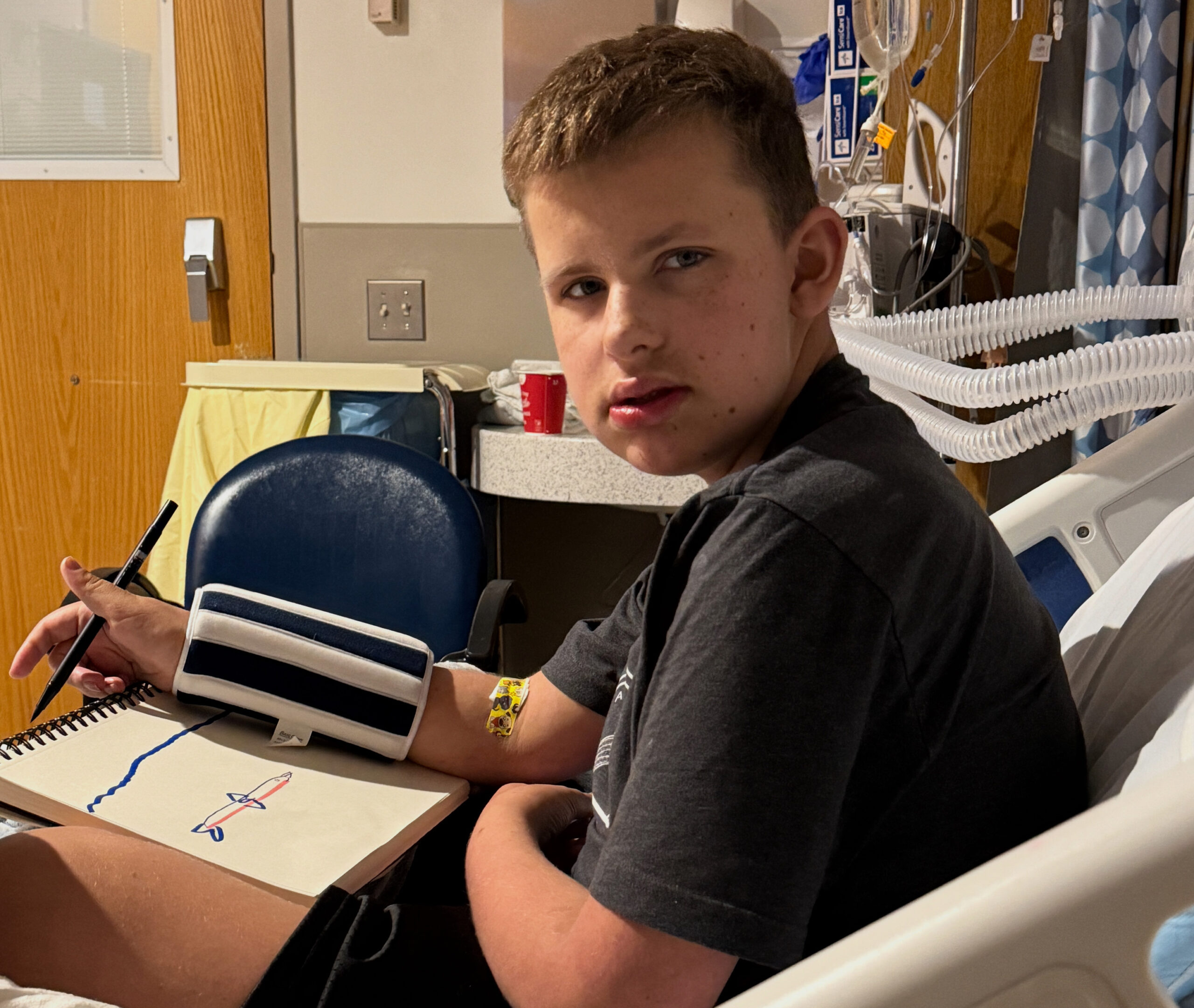
Hope for HO – a mother shares her experiences in finding a solution for her son’s HO.
HO Clinical Trials Panel – a recent panel of principle investigators on promising treatments for HO.
Hungry for Solutions, Marci Serota, RDN This book was written by a mother and registered dietician sharing her quest to find solutions for her son with HO.
Would You Know How to Recognize and Treat Hypothalamic Obesity?
Marci Serota, RDN with Eugenie Hsu, PhD and Shana McCormack, MD, MTR
Feasibility, safety, and efficacy of dietary or lifestyle interventions for hypothalamic obesity: A systematic review.
Van Roessel IMAA, Van Den Brink M, Dekker J, Ruitenburg-van Essen BG, Tissing WJE, van Santen HM. Clin Nutr. 2024 May 27;43(8):1798-1811. doi: 10.1016/j.clnu.2024.05.028. Online ahead of print. PMID: 38955055
Zhang Q, Feng Y, Wu D, Xie Y, Wu G, Wu W, Wang H, Liu X, Fan L, Xiang B, Sun Q, Li Y, Wang Y, Ye H. Serum Metabolomic and Lipidomic Profiling Reveals the Signature for Postoperative Obesity among Adult-Onset Craniopharyngioma. Metabolites. 2024 Jun 17;14(6):338. doi: 10.3390/metabo14060338. PMID: 38921473; PMCID: PMC11205291.
Beckhaus J, Eveslage M, Bison B, Friedrich C, Müller HL. Impact of parental body mass index at diagnosis on obesity in survivors of pediatric craniopharyngioma. Endocr Connect. 2024 Jun 1:EC-24-0126. doi: 10.1530/EC-24-0126. Epub ahead of print. PMID: 38904467.
Müller HL, Zhou J, Peng J. Editorial: Recent advances in pediatric craniopharyngioma. Front Endocrinol (Lausanne). 2024 Apr 19;15:1413744. doi: 10.3389/fendo.2024.1413744. PMID: 38706703; PMCID: PMC11066279.
Roth CL, Scimia C, Shoemaker AH, Gottschalk M, Miller J, Yuan G, Malhotra S, Abuzzahab MJ. Setmelanotide for the treatment of acquired hypothalamic obesity: a phase 2, open-label, multicentre trial. Lancet Diabetes Endocrinol. 2024 Jun;12(6):380-389. doi: 10.1016/S2213-8587(24)00087-1. Epub 2024 Apr 30. PMID: 38697184.
Tena-Sempere M. Setmelanotide: new promise for the treatment of hypothalamic obesity? Lancet Diabetes Endocrinol. 2024 Jun;12(6):366-367. doi: 10.1016/S2213-8587(24)00109-8. Epub 2024 Apr 30. PMID: 38697183.
Rovani S, Butler V, Samara-Boustani D, Pinto G, Gonzalez-Briceno L, Nguyen Quoc A, Vermillac G, Stoupa A, Besançon A, Beltrand J, Thalassinos C, Flechtner I, Dassa Y, Viaud M, Arrom-Branas MB, Boddaert N, Puget S, Blauwblomme T, Alapetite C, Bolle S, Doz F, Grill J, Dufour C, Bourdeaut F, Abbou S, Guerrini-Rousseau L, Leruste A, Beccaria K, Polak M, Kariyawasam D. Long-term weight gain in children with craniopharyngioma. Eur J Endocrinol. 2024 May 2;190(5):363-373. doi: 10.1093/ejendo/lvae044. PMID: 38662730.
Tsumori M, Itonaga T, Oyake M, Hirano N, Oyama N, Ihara K. Infantile Hypothalamic Hamartoma: A Rare Presentation of Isolated Obesity. JCEM Case Rep. 2024 Mar 19;2(3):luae033. doi: 10.1210/jcemcr/luae033. PMID: 38505090; PMCID: PMC10948354.
Chartoumpekis DV, Habeos EE, Psilopanagioti A. Evaluating the effectiveness and underlying mechanisms of incretin-based treatments for hypothalamic obesity: A narrative review. Obes Pillars. 2024 Feb 24;10:100104. doi: 10.1016/j.obpill.2024.100104. PMID: 38463533; PMCID: PMC10924130.
Roth CL, McCormack SE. Acquired hypothalamic obesity: A clinical overview and update. Diabetes Obes Metab. 2024 Apr;26 Suppl 2:34-45. doi: 10.1111/dom.15530. Epub 2024 Mar 7. PMID: 38450938.
Gatta-Cherifi B, Mohammedi K, Cariou T, Poitou C, Touraine P, Raverot G, Brue T, Chanson P, Illouz F, Grunenwald S, Chabre O, Sonnet E, Cuny T, Bertherat J, Czernichow S, Frison E, Tabarin A. Impact of exenatide on weight loss and eating behavior in adults with craniopharyngioma-related obesity: the CRANIOEXE randomized placebo-controlled trial. Eur J Endocrinol.
Pereira Neto B, Pais Cunha I, Leite-Almeida AL, Ferreira S, Coelho J, Lago R, Pereira J, Gil-da-Costa MJ, Almeida P, Castro-Correia C. Quality of Life and Hormonal Impairment in Pediatric Patients With Craniopharyngiomas. Cureus. 2024 Jan 20;16(1):e52621. doi: 10.7759/cureus.52621. PMID: 38374867; PMCID: PMC10875977.
Ng VWW, Gerard G, Koh JJK, Loke KY, Lee YS, Ng NBH. The role of glucagon-like peptide 1 receptor agonists for weight control in individuals with acquired hypothalamic obesity-A systematic review. Clin Obes. 2024 Jun;14(3):e12642. doi: 10.1111/cob.12642. Epub 2024 Jan 25. PMID: 38273176.
van Santen HM, Denzer C, Müller HL. Could setmelanotide be the game-changer for acquired hypothalamic obesity? Front Endocrinol (Lausanne). 2024 Jan 4;14:1307889. doi: 10.3389/fendo.2023.1307889. PMID: 38239988; PMCID: PMC10794340.
Gan HW, Cerbone M, Dattani MT. Appetite- and Weight-Regulating Neuroendocrine Circuitry in Hypothalamic Obesity. Endocr Rev. 2024 May 7;45(3):309-342. doi: 10.1210/endrev/bnad033. PMID: 38019584; PMCID: PMC11074800.
Roth CL, Zenno A.Treatment of hypothalamic obesity in people with hypothalamic injury: new drugs are on the horizon. Front Endocrinol (Lausanne). 2023 Sep 13;14:1256514. doi: 10.3389/fendo.2023.1256514. PMID: 37780616; PMCID: PMC10533996.
Hu HZ, Lei L. Bariatric surgery for hypothalamic obesity in patients with craniopharyngioma: A literature review. Asian J Surg. 2023 Dec;46(12):5479. doi: 10.1016/j.asjsur.2023.07.117. Epub 2023 Aug 1. PMID: 37537035.
Dassen AR, van Schaik J, van den Munckhof P, Schuurman PR, Hoving EW, van Santen HM. Could deep brain stimulation be a possible solution for acquired hypothalamic obesity? Heliyon. 2023 Mar 9;9(3):e14411. doi: 10.1016/j.heliyon.2023.e14411. PMID: 36967879; PMCID: PMC10036662
Sciacovelli C, Moschione G, Garelli S, Pagotto U. Semaglutide for Treating Obesity Induced by Craniopharyngioma Resection: A Successful Case Study. JCEM Case Rep. 2023 Jul 27;1(4):luad074. doi: 10.1210/jcemcr/luad074. PMID: 37908981; PMCID: PMC10580492.
Yousuf OK, Salehani A, Zimmerman K, Estevez-Ordonez D, Madura C, Arynchyna-Smith A, Johnston JM, Rozzelle CJ, Rocque BG, Blount JP. Does subtotal resection ameliorate hypothalamic morbidity in pediatric craniopharyngioma? A 30-year retrospective cohort study. J Neurosurg Pediatr. 2023 Aug 11;32(5):569-575. doi: 10.3171/2023.5.PEDS22568.
van Roessel IMAA, de Graaf JP, Biermasz NR, Charmandari E, van Santen HM. Acquired hypothalamic dysfunction in childhood: ‘what do patients need?’ – an Endo-ERN survey. Endocr Connect. 2023 Sep 13;12(10):e230147. doi: 10.1530/EC-23-0147. PMID: 37531603; PMCID: PMC10503223.
Kayadjanian N, Hsu EA, Wood AM, Carson DS. Caregiver Burden and Its Relationship to Health-Related Quality of Life in Craniopharyngioma Survivors. J Clin Endocrinol Metab. 2023 Dec 21;109(1):e76-e87. doi: 10.1210/clinem/dgad488. PMID: 37597173; PMCID: PMC10735386.
Van Schaik J, Schouten-van Meeteren AYN, Vos-Kerkhof E, Janssens GO, Porro GL, Fiocco M, Bakker B, Tissing WJE, Hoving EW, van Santen HM. Treatment and outcome of the Dutch Childhood Craniopharyngioma Cohort study: First results after centralization of care. Neuro Oncol. 2023 Dec 8;25(12):2250-2261. doi: 10.1093/neuonc/noad112. PMID: 37381692; PMCID: PMC10708930.
Schultes B, Ernst B. Long-term outcomes after gastric bypass surgery in patients with craniopharyngioma-related hypothalamic obesity-Three cases with 7, 8, and 14 years follow-up. Obes Res Clin Pract. 2023 Jul-Aug;17(4):361-365. doi: 10.1016/j.orcp.2023.06.004. Epub 2023 Jun 26. PMID: 37380506.
Hinton EC, Lithander FE, Elsworth RL, Hawton K, Narayan K, Szymkowiak S, Bedford HL, Naeem N, Elson R, Taylor-Miller T, Hamilton-Shield JP, Crowne EC. Evaluating Eating Behaviour, Energy Homeostasis, and Obesity in Childhood-Onset Craniopharyngioma: A Feasibility Study. Horm Res Paediatr. 2024;97(1):80-93. doi: 10.1159/000530863. Epub 2023 May 17. PMID: 37231854; PMCID: PMC10777714
McCormack SE, Wang Z, Wade KL, Dedio A, Cilenti N, Crowley J, Plessow F, Bamba V, Roizen JD, Jiang Y, Stylli J, Ramakrishnan A, Platt ML, Shekdar K, Fisher MJ, Vetter VL, Hocking M, Xiao R, Lawson EA. A Pilot Randomized Clinical Trial of Intranasal Oxytocin to Promote Weight Loss in Individuals With Hypothalamic Obesity. J Endocr Soc. 2023 Mar 17;7(5):bvad037. doi: 10.1210/jendso/bvad037. PMID: 37153702; PMCID: PMC10154909.
Beckhaus J, Friedrich C, Boekhoff S, Calaminus G, Bison B, Eveslage M, Timmermann B, Flitsch J, Müller HL. Outcome after pediatric craniopharyngioma: the role of age at diagnosis and hypothalamic damage. Eur J Endocrinol. 2023 Mar 2;188(3):lvad027. doi: 10.1093/ejendo/lvad027. PMID: 36857103
Rachmasari KN, Strauss SB, Phillips CD, Lantos JE, An A, Cisse B, Ramakrishna R, Schwartz TH, Dobri GA. Posterior hypothalamic involvement on pre-operative MRI predicts hypothalamic obesity in craniopharyngiomas. Pituitary. 2023 Feb;26(1):105-114. doi: 10.1007/s11102-022-01294-0. Epub 2022 Dec 3. PMID: 36462067.
Shoemaker AH, Tamaroff J. Approach to the Patient With Hypothalamic Obesity. J Clin Endocrinol Metab. 2023 Apr 13;108(5):1236-1242. doi: 10.1210/clinem/dgac678. PMID: 36413492; PMCID: PMC10306088.
Craven M, Crowley JH, Chiang L, Kline C, Malbari F, Hocking MC, McCormack SE. A Survey of Patient-Relevant Outcomes in Pediatric Craniopharyngioma: Focus on Hypothalamic Obesity. Front Endocrinol (Lausanne). 2022 May 9;13:876770. doi: 10.3389/fendo.2022.876770. PMID: 35615720; PMCID: PMC9124861.
Oxytocin and Naltrexone Successfully Treat Hypothalamic Obesity in a Boy Post-Craniopharyngioma Resection
Eugenie A Hsu, Jennifer L Miller, Francisco A Perez, Christian L Roth
Hypothalamic Obesity: Prologue and Promise
Abuzzahab M.J.a, Roth C.L.b, Shoemaker A.H.c
A Pilot Randomized Clinical Trial of Intranasal Oxytocin to Promote Weight Loss in Individuals With Hypothalamic Obesity
Shana E McCormack, Zi Wang, Kristin L Wade, Anna Dedio, Nicolette Cilenti, Julia Crowley, Franziska Plessow, Vaneeta Bamba, Jeffrey D Roizen, Yaoguang Jiang, Jack Stylli, Arjun Ramakrishnan, Michael L Platt, Karuna Shekdar, Michael J Fisher, Victoria L Vetter, Matthew Hocking, Rui Xiao, Elizabeth A Lawson
Connect With Us
If you’re a clinician, researcher, or industry partner working to improve outcomes in acquired hypothalamic obesity, we’d love to hear from you.
Whether you’re looking to:
- Refer a patient to our support programs or resources
- Learn more about our patient registry and real-world data
- Collaborate on research or clinical trial engagement
- Access caregiver insights or advocacy tools
We welcome the opportunity to partner with you.
Email us at outreach@rawoodfoundation.org
Encourage Your Patients to Join the Hypothalamic-Pituitary Brain Tumors Patient Registry
Help advance understanding of acquired hypothalamic obesity and hypothalamic-pituitary tumors by encouraging your patients to enroll in the RAWF Patient Registry.This secure, longitudinal registry captures real-world experiences, treatment outcomes, and quality-of-life data directly from patients and caregivers. The insights gained help inform clinical practice, guide research priorities, and support advocacy for better treatments.

Hypothalamic Obesity News
Hypothalamic Syndrome: Finally, a Way to Describe What We’ve Been Living

New Frontiers in Hypothalamic Obesity Research
Updates on Current and Pending Hypothalamic Obesity Clinical Trials

Raymond A. Wood Foundation Partners with STOP Obesity Alliance
Support Our Work
The Raymond A. Wood Foundation advocates for survivors and caregivers faced with challenges after brain tumor treatment. A donation — big or small — helps us do this important work.

